Researchers at the University of São Paulo (USP) in Brazil have found that severe COVID-19 is associated with an imbalance in an important immune system signaling pathway. The discovery helps explain at the molecular level why some people infected by SARS-CoV-2 develop a potentially fatal systemic inflammation. It also paves the way to the development of more specific therapies.
An article on the study, which was funded by FAPESP, is published in Frontiers in Immunology.
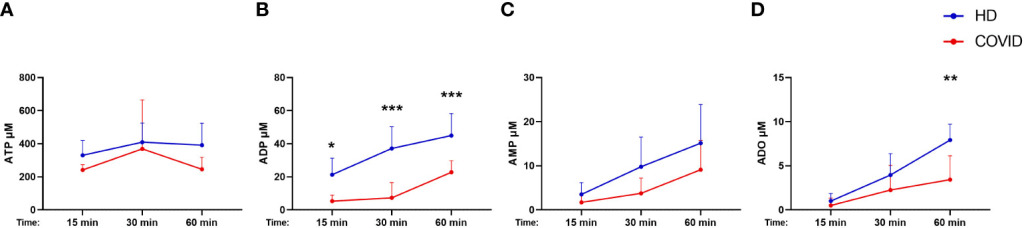
The researchers detected dysregulation of the immune system mediated by ATP (adenosine triphosphate), one of the main sources of energy for cellular processes. Severe COVID-19 patients had higher levels of ATP in their blood and lower levels of adenosine, which should increase when ATP is metabolized for energy production.
“The immune system comprises several signaling pathways that provide alerts in response to invasion by a pathogen, for example. One involves ATP, which triggers the release of inflammatory substances in defense cells to attack the invader. The immune system also has control mechanisms to avoid excessive inflammation, but when this error in ATP metabolization occurs, it results in a huge imbalance and systemic dysfunctions in the immune response,” said Maria Notomi Sato, a professor at USP’s Medical School and last author of the article.
The increase in unmetabolized ATP, according to the article, produces a pro-inflammatory state and triggers a potentially fatal systemic inflammation known as a cytokine storm. “The study pointed to an imbalance in the signaling system and a dysfunction in the regulation of these components, as one more factor at the systemic level that attacks the organs of severe COVID-19 patients,” Sato said.
ATP is constantly produced by cells and is broken down in the extracellular environment by enzymes called ectonucleotidases. “ATP turns into a danger signal when it exits cells in large amounts. When does that happen? When an exacerbated inflammatory response is activated, when cells are badly injured or when some other severe damage occurs. In response, ATP triggers an inflammatory process that involves other cells in a chain reaction,” said Anna Julia Pietrobon, first author of the article. She is a PhD candidate at the Virology Institute of Charité University Hospital Berlin in Germany.
Alteration in metabolization of ATP to adenosine
In the study, the researchers measured ATP and adenosine levels in blood samples from 88 severe COVID-19 patients collected in 2020-21. None of the patients had been vaccinated.
“We found cell-surface ectonucleotidases that cleave ATP to be less expressed in cells from both mild and severe COVID-19 patients, but particularly the latter. In fact, we concluded that the higher the ATP level, the more severe the disease,” Pietrobon said.
The researchers also investigated possible alterations in immune system cells. “We found that some immune cells, especially B lymphocytes, expressed less CD39 and CD73, enzymes that break down ATP. Lymphocyte levels generally tend to be low in COVID-19 patients, but in our study not only the levels of B cells in blood from severe patients were low, but these cells also expressed lower amounts of both enzymes, contributing to less ATP metabolization and hence less production of adenosine, the anti-inflammatory component that would try to regulate this response,” Pietrobon said.
Given this finding, the researchers decided to isolate the B cells present in the blood samples and provide them with ATP. “We conducted an in vivo experiment in which we gave ATP to cells from both COVID-19 patient and healthy controls. The B cells from patients produced less adenosine than those from the healthy controls, possibly because they expressed less CD39 and CD73,” she said.
It should be noted that the researchers do not yet know if the alteration in ATP metabolization causes or is caused by the exacerbated inflammatory response to SARS-CoV-2. They plan to investigate this in future projects.
Systemic reaction
A study conducted at the Center for Research on Inflammatory Diseases (CRID) had already detected a link between severe COVID-19 and inflammasome activation, which in these patients is exacerbated and fails to shut down after the infection clears (read more at: agencia.fapesp.br/39411).
CRID is a Research, Innovation and Dissemination Center (RIDC) funded by FAPESP and hosted by USP’s Ribeirão Preto Medical School.
The inflammasome is a protein complex inside defense cells. When this cellular mechanism is activated, pro-inflammatory molecules known as cytokines are produced to warn the immune system that more defense cells need to be sent to the infection site.
According to the researchers who conducted the study on ATP metabolization, the build-up of ATP in conjunction with low levels of adenosine in severe patients may contribute to exacerbation of the cytokine-mediated inflammatory response. “The inflammatory process triggered by insufficient ATP breakdown occurs because of decompensation in this pathway, which functions as a form of anti-inflammatory regulation. However, when this error in the ATP-adenosine metabolism occurs, the ATP build-up acts as a signal to other inflammation pathways in the immune system, culminating in inflammasome activation, for example,” Sato said
In these cases, in which immune system regulation is dysfunctional, the excessive inflammatory response is directly linked to multiple organ failure and frequently to death.
The article “Dysfunctional purinergic signaling correlates with disease severity in COVID-19 patients” is at: www.frontiersin.org/articles/10.3389/fimmu.2022.1012027/full.

Leave a Reply